AMH and Its Role in Female Fertility
Anti-Müllerian Hormone (AMH) is a hormone produced by the ovarian follicles that reflects the ovarian reserve. In simpler terms, it indicates how many eggs remain in the ovaries. AMH is considered one of the most reliable markers to assess fertility potential because it does not vary drastically during the menstrual cycle. For Indian women, AMH testing has become a standard part of infertility evaluation due to rising delays in childbearing and lifestyle changes.
Why AMH Matters
It predicts ovarian response during IVF or IUI cycles.
It helps identify diminished ovarian reserve.
It assists doctors in planning stimulation protocols.
It offers insights into menopause timelines.
What Is Considered a Low AMH Level
While normal AMH ranges vary by age, Indian fertility clinics commonly use the following reference chart.
| AMH Level (ng/mL) | Interpretation | Clinical Meaning |
|---|---|---|
| Above 3.0 | High | Strong ovarian response |
| 1.2 – 3.0 | Normal | Good ovarian reserve |
| 0.5 – 1.1 | Low | Reduced egg count |
| Below 0.5 | Very Low | Severe reduction in ovarian reserve |
A value below 1.1 ng/mL is generally considered low. However, prognosis depends on age, egg quality, hormonal balance, and overall reproductive health.
Common Causes Behind Low AMH Levels
Low AMH is a multifactorial condition. Some causes are age-related, while others are medical or lifestyle-induced.
Age: AMH naturally declines with age, especially after 33 and more rapidly after 35.
Genetics: Family history of early menopause can predispose women to a lower ovarian reserve.
Medical Conditions
Endometriosis
Autoimmune disorders
Chromosomal abnormalities
Premature ovarian insufficiency
Lifestyle Factors
Smoking
Severe stress
Nutritional deficiencies
Long-term exposure to environmental toxins
Symptoms and Early Warning Signs
Low AMH does not show obvious external symptoms. However, some indicators may suggest diminished ovarian reserve.
Irregular Menstrual Cycles: Shorter cycles or unpredictable ovulation patterns.
Poor Response to Fertility Medication: Women with low AMH often produce fewer follicles during stimulation cycles.
Difficulty Conceiving Naturally: Reduced egg quantity and quality may make conception harder.
Early Menopause Tendencies: In severe cases, low AMH may signal an earlier menopause.
How Low AMH Is Diagnosed
Low AMH is diagnosed through a combination of blood tests and ultrasound scans. The AMH blood test is done on any day of the menstrual cycle and helps assess ovarian reserve. Doctors also perform an Antral Follicle Count (AFC) through a transvaginal ultrasound to measure the number of small follicles in the ovaries. Additional hormone tests such as FSH, Estradiol, LH, thyroid profile, and prolactin help determine whether low AMH is connected to broader hormonal imbalances. Together, these tests give clarity on ovarian function and guide treatment planning.
Prognosis: What Low AMH Means for Fertility
Low AMH reflects a reduced egg count but does not mean that pregnancy is impossible. Many women with low AMH still conceive naturally or with fertility support. Prognosis depends on age, egg quality, underlying conditions like PCOS or endometriosis, lifestyle habits, and how long conception has been attempted. Data from Indian fertility centres shows that women under 35 with AMH between 0.5 and 1.1 can still respond well to IVF when stimulation protocols are customized.
Treatment Approaches for Low AMH
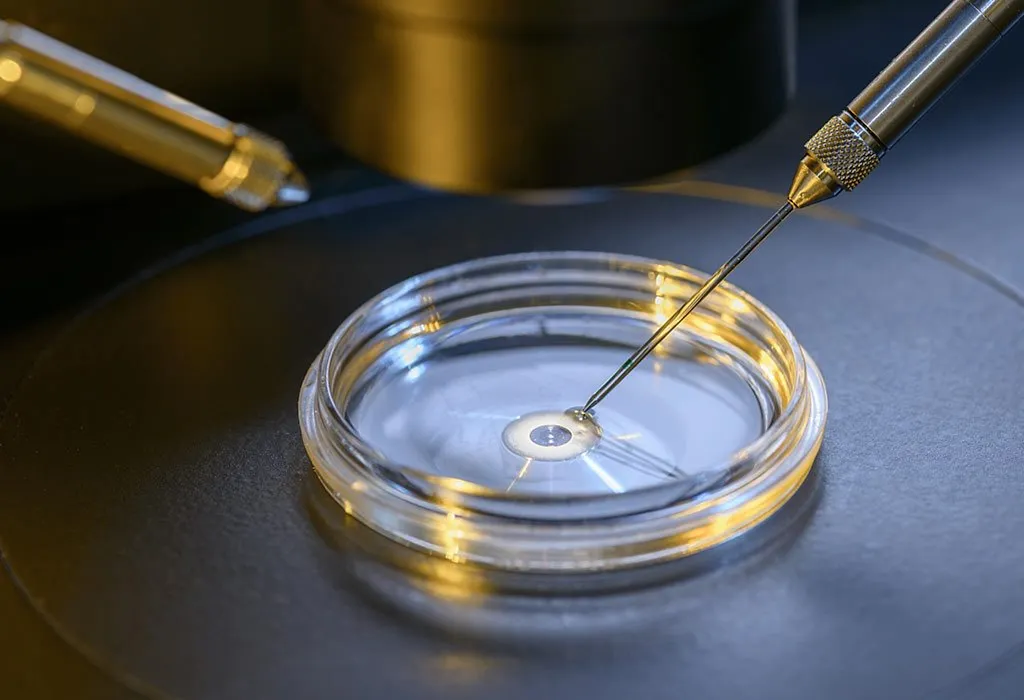
Treatment focuses on maximizing egg quality and optimizing the response to fertility medications. Ovulation induction helps women attempting natural conception or IUI. IVF becomes the preferred option when egg reserve is lower, with success depending more on egg quality than quantity. Donor egg IVF is recommended in cases of extremely low AMH or failed cycles. For women wishing to delay pregnancy, egg freezing allows preservation of eggs while they are still viable.
Personalized Fertility Plans for Women with Low AMH
Personalized plans help improve outcomes. Customized ovarian stimulation adjusts medication doses based on AMH and AFC. Dual stimulation protocols allow egg retrieval twice in one menstrual cycle, increasing the number of eggs collected. Minimal stimulation IVF uses lower medication doses to avoid ovarian fatigue in women with very low AMH. Sequential cycle IVF gathers eggs over multiple cycles to improve embryo formation chances.
Lifestyle and Dietary Support Backed by Research
Lifestyle changes do not increase AMH but support egg quality and hormone balance. A diet rich in antioxidants helps protect eggs from stress. Omega-3 fatty acids assist hormonal regulation. Stress-reducing practices such as yoga and meditation can improve ovulation. Maintaining healthy body weight and avoiding toxins further supports reproductive health.
| Intervention | Benefit |
|---|---|
| High-antioxidant diet | Improves egg quality |
| Omega-3 fatty acids | Supports hormone balance |
| Stress reduction methods | Regulates ovulation |
| Weight management | Enhances IVF outcomes |
| Avoiding toxins | Protects ovarian health |
Supplements such as CoQ10, DHEA (with medical supervision), Vitamin D, and folate may support egg health and hormonal balance.
Comparing Treatment Outcomes
Success rates vary based on age, AMH levels, and treatment type. Younger women generally have better outcomes even with low ovarian reserve. A comparison from Indian fertility data is shown below.
| Age Group | Clinical Pregnancy Rate |
|---|---|
| Below 30 | 35 to 45 percent |
| 30–34 | 30 to 40 percent |
| 35–37 | 20 to 30 percent |
| 38–40 | 15 to 20 percent |
| Above 40 | 5 to 10 percent |
When to Consult a Fertility Specialist
A specialist should be consulted if conception has not occurred within six months, especially after age 30. Irregular periods, family history of early menopause, conditions like endometriosis, or plans to conceive after 35 are also reasons to seek early evaluation. Timely intervention improves overall prognosis and expands treatment options.